Research Terms
Preston A. Wells, Jr. Center for Brain Tumor Therapy
| Director |
William Friedman Duane Mitchell |
| Phone | 352-273-9000 |
| Website | https://braintumors.ufhealth.org/?utm_source=bing&utm_medium=tj%20ppc&msclkid=e9deb304b725153d50daee9b341bf036 |
| Mission | The mission of the Preston A. Wells, Jr. Brain Tumor Therapy Center at the University of Florida (BTTC) is to create one of the top ten comprehensive brain tumor therapy centers in the United States. The purpose of such a comprehensive cneter is to treat and, hopefully, cure brain and spinal cord tumors in adults and children. Specific goals follow: 1) Conduct bench and clinical research leading to the cure of brain and spinal cord tumors. 2) Establish and implement educational opportunities for medical professionals, scientists, patients, and families. 3) Provide a world-class comprehensive brain tumor therapy center for the citizens of the State of Florida. |
Clinical and Translational Science Institute
| Director |
Elizabeth Shenkman Duane Mitchell |
| Phone | 352-273-8700 |
| Website | https://ctsi.ufl.edu |
| Mission | The University of Florida has a rich environment of distinguished colleges, state-of-the-art research facilities and statewide health education and health delivery systems. These resources position UF at the forefront of institutions to train the next generation of clinical and translational investigators and to help overcome two major obstacles in our nation's clinical research enterprise: the translation of basic science discoveries to early investigations in humans and the translational of clinical research into better medical practice and healthcare delivery. UF has made considerable investments dedicated exclusively to accomplish these missions through the creation of a trans-institutional Clinical and Translational Science Institute (CTSI). The institute will provide the new intellectual home for clinical and translational research and training at UF, integrating and synergizing the scientific and educational activities of 16 colleges, two academic and clinical campuses, three regional healthcare systems and the 67 counties of the State of Florida. |
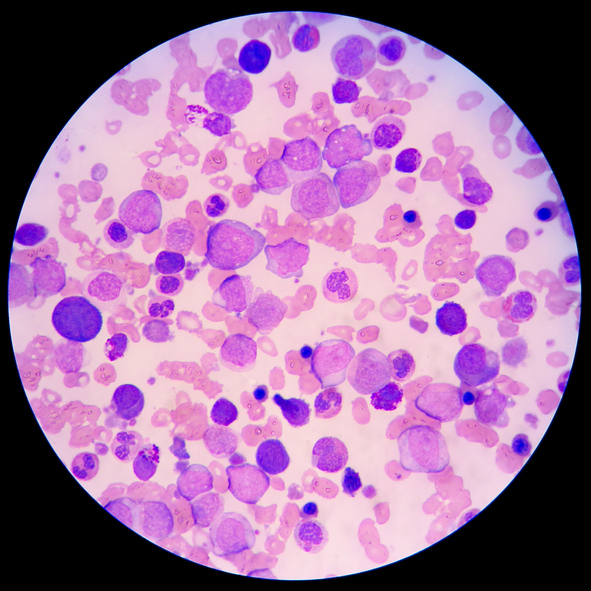
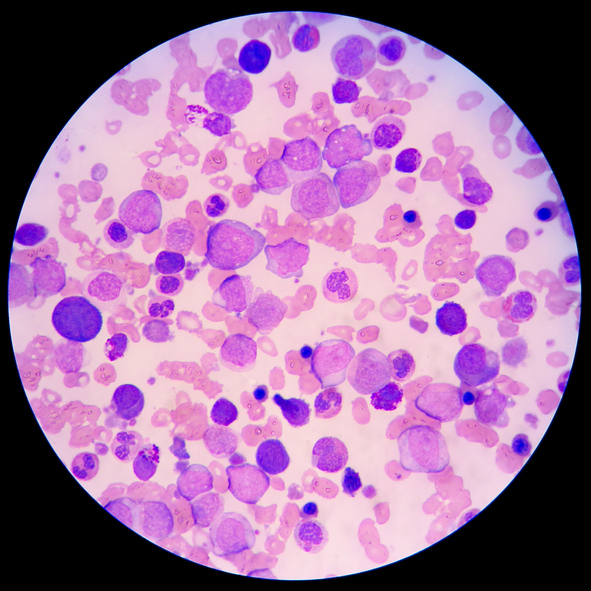
This nanoparticle vaccine targets the slow-cycling, treatment-resistant, cancer stem cells to improve efficiency of anti-cancer drugs, thereby improving disease prognosis. Despite major developments in the field of anti-cancer therapies, tumor recurrence and metastasis after chemotherapy is still the major cause of cancer patient mortality. Although current RNA-lipid nanoparticle (NP) vaccines have shown promising results, they still remain encumbered by profound intra-tumoral and systemic immunosuppression. Because of the heterogeneity of cancer epitopes, a major challenge in the field of vaccine development is determining the best target. Studies carried out by our researchers at the University of Florida have demonstrated that recurrences in gliomas can be attributed to the subset of slowly dividing cells, resistant to conventional anti-cancer therapies. These slowly dividing cells exhibit enhanced tumorigenicity and infiltrative propensity. Hence, clinical strategies targeting this specific population of cancer cells holds great potential in improving therapeutic efficiency of drugs.
To address this issue of cancer recurrence, our scientists have developed a universal RNA-NP vaccine engineered with RNAs for epitopes specific to slow-cycling tumor cells, as well as a personalized RNA-NP vaccine engineered from RNA extracted from patient’s tumor biopsy. These vaccines are able to activate T-cell recognition of slow-cycling tumor-initiating stem cells mediating sustained anti-tumor activity in the mouse model of glioma.
Nanoparticle vaccine for either personalized or universal treatment of cancer
This therapeutic platform demonstrates the use of two different nanoparticle (NP) vaccines (personalized and universal) engineered with RNA derived from a specific subpopulation of slow-cycling, tumor-initiating stem cells. These immunomodulating vaccines are able to elicit T-cell response against slow-cycling, tumor-initiating cancer stem cells, leading to sustained anti-tumor activity. Researchers found that systemic administration of this vaccine primes the peripheral and intra-tumoral microenvironments for response to immunotherapy. These RNA-NPs localize to heart, lung, bone marrow, spleen, liver, kidney and subcutaneous/intracranial tumors. In immunologically resistant tumor models (i.e. B16F0, B16-F10, Lewis lung carcinoma) resistant to immune checkpoint inhibitors, these RNA-NPs activate the preponderance of systemic and intra-tumoral antigen presenting cells (characterized by co-expression of PD-L1 and CD86) for induction of anti-tumor immunity. Altogether, this therapeutic platform delivers specific sets of tumor RNA antigens purified from slow-cycling cancer stem cells to create personalized or universal vaccines.
This cancer vaccine activates antigen-presenting cells and induces anti-tumor immune system activity for the treatment of diffuse intrinsic pontine gliomas (DIPG). DIPG tumors originate in the pons, an area of the brainstem controlling vital body functions such as breathing and heart rate. DIPG is the main type of brain tumor causing death in children, and it comprises 10-20 percent of all pediatric brain tumor cases. The widely spread nature and location of these tumors prevent early diagnosis, which greatly limits treatment options. Surgical resection is not possible due to the tumors’ location, and chemotherapy has not been successful at treating DIPG. Radiation therapy has been able to shrink tumor size, but this effect is typically short-lived and does not cure patients. Diagnosing patients with DIPG usually occurs between the ages of 5 and 9, and their median survival rate is 10-11 months.
Researchers at the University of Florida have developed a vaccine that treats DIPG by driving anti-tumor immunity. The global RNA therapeutics and vaccine market is expected to surpass $800 million by the end of 2029. This RNA vaccine delivers liposomal nanoparticles by intravenous injection that activate specific antigen-presenting cells to increase immunogenicity against DIPG. Improved survival rates in animal models have demonstrated the vaccine’s success.
An off-the-shelf vaccine for the treatment of diffuse intrinsic pontine glioma (DIPG)
This RNA vaccine targets a homogenously expressed diffuse intrinsic pontine glioma (DIPG) tumor antigen, allowing for widespread use without the need for customized treatment. The RNA renewably encodes specific DIPG antigens to continuously vaccinate the patient, increasing central memory T-cell levels for sustained anti-tumor immunity. A liposomal nanoparticle delivers the vaccine to prevent RNA degradation.
This micro-biofabrication system combines computer vision, robotics, micromanipulation tools, and a novel culture medium to enable the creation of optimized 3D cellular structures. A level of exquisite detail exists in the intricate pattern and spatial structure of cells found in developing tissue. Micromanipulation tools allow precise translation and placement of single cells. However, available bioprinting systems cannot employ these tools to build highly intricate multicellular 3D structures in a cell-by-cell manner. They cannot hold the deposited cells in place while building structures without creating misconfigured layers or dispersed single cells. Researchers in many fields need effectively perfect multicellular 3D structures to understand topics like embryonic development, function-form relationships, immune signaling, and drug screening for efficacy and toxicity.
Researchers at the University of Florida have developed a cellular micro-masonry system that enables the microfabrication of highly intricate 3D cell structures. A 3D printing culture medium supports cellular structures as they are built one cell at a time using micromanipulation techniques and real-time imaging.
A bioprinting system that builds perfect 3D structures cell by cell
This cellular micro-masonry system integrates a cell translation system, an imaging system, and a 3D culture medium. The culture medium that supports the 3D construction of cells is a liquid-like solid made from jammed microgels swollen in liquid growth media. Through micromanipulation and cell aspiration performed within this culture medium, the system retrieves dispersed cells one at a time, translates them to the building area, and places them at the desired location in 3D space. The system is mounted on a fast-scanning multi-photon microscope to enable real-time tracking of cells, path corrections, and structural refinements during the building process.
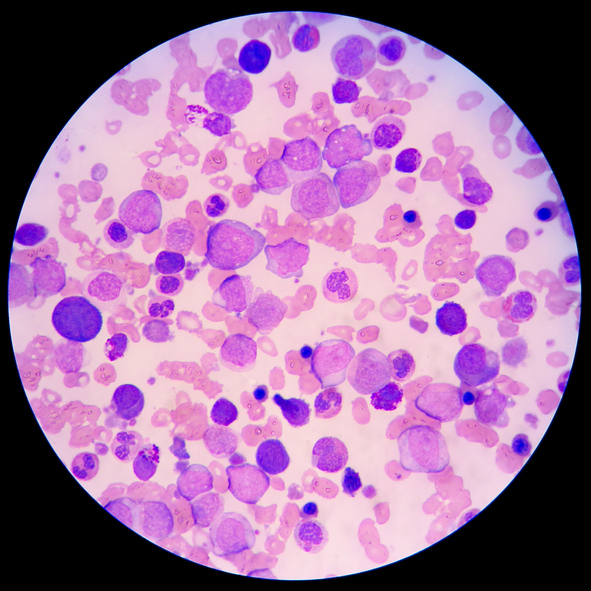
These sarcosine-loaded dendritic cells exhibit enhanced migration to local lymph nodes, increasing the stimulation and migration of T-cells for cancer treatment. Immunotherapy has become a popular approach to treat cancer in recent years. A particular approach is providing patients with a vaccine of their own dendritic cells that presents a particular tumor antigen. University of Florida researchers have developed dendritic cells loaded intracellularly with sarcosine. Sarcosine, also known as N-methylglycine, is a metabolite of an amino acid found naturally in biological tissues; it is easily acquired from a variety of companies. The dendritic cells containing sarcosine have shown to significantly improve dendritic cell migration, in turn increasing stimulation of an immune response, resulting in the tumor being attacked and killed. Using dendritic cells for tumor treatment has already been approved by the FDA in prostate cancer and is currently in phase III clinical trials for other forms of cancers.
Sarcosine-loaded dendritic cells used for adoptive immunotherapy increases immune response and potentially survival rate of cancer patients
Dendritic cells act as antigen presenting cells (APCs), presenting antigens to T-cell receptors. One immunotherapy approach to treating cancer provides patients with a vaccine of their own dendritic cells loaded with tumor antigens. Those dendritic cells migrate to a lymph node where they simulate T cells to generate an immune response, allowing the cells to express the target antigen that results in tumor killing. Enhancing that migration of dendritic cells to the local lymph node is critical for efficacy of this treatment strategy. University of Florida researchers have discovered that loading those dendritic cells with sarcosine, a common metabolite, significantly improves migration to local lymph nodes compared to previous strategies. This sarcosine addition for treatment can be applied to other cells such as T-cells in an adoptive immunotherapy strategy. This intracellular sarcosine loading method also has the potential to enhance migration of T-cells and stem cells allowing this treatment to be applicable in other diseases.
This therapeutic vaccine treats Lewy body diseases, such as Parkinson’s disease, by clearing misfolded protein aggregates utilizing a patient's own immune system. An estimated 1.4 million people in the U.S. suffer from Lewy body dementia, making it the second most frequent form of degenerative dementia in the country. However, Lewy body diseases often go misdiagnosed until patients present symptoms associated with moderate or severe stages of the disease. Incorrectly prescribed medications due to misdiagnosis further worsens the disease state, potentially resulting in death. Available treatments for Lewy body diseases include a peptide-based vaccine under clinical trial investigation. However, the use of peptide and related antibody-inducing vaccines runs the risk of prompting an auto-immune response in the patient. Other treatment options for these diseases provide only symptomatic relief that wears off as the disease progresses and does nothing to prevent further neurodegeneration.
Researchers at the University of Florida have developed an adoptive cellular therapy vaccine that makes use of the patient’s own cellular immunity to reduce the misfolded protein aggregates characteristic of Lewy body diseases, providing treatment by inhibiting future neurodegeneration. Since this vaccine does not involve the use of antibodies, the chance of patients experiencing an auto-immune response decreases.
Adoptive cellular therapy vaccine that treats Lewy body diseases with lessened risk of auto-immune response
This adoptive cellular therapy involves taking T cells from the patient’s body, exposing them to an alpha-synuclein mutant antigen, and administering the T cells back into the patient’s body. This grants the patient’s immune system the ability to specifically target cells containing the misfolded alpha-synuclein aggregates and clear them from the body, preventing accumulation of the mutant proteins.
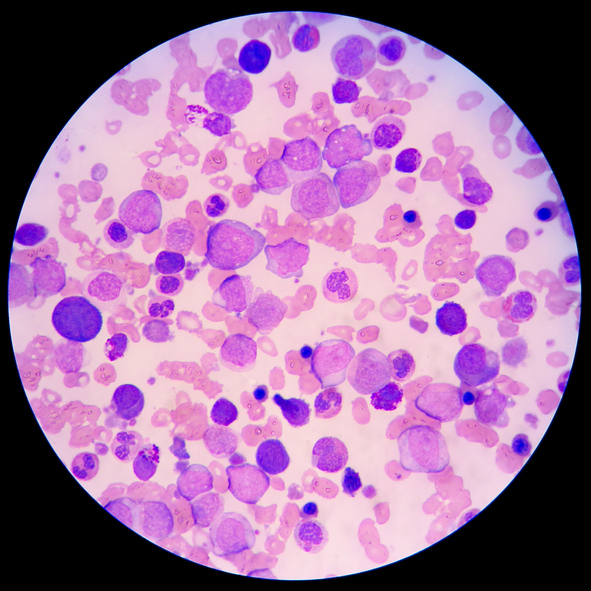
This T cell-based immunotherapy aims to enhance anti-tumor immune response by addressing metabolic restrictions within tumor microenvironments. T cells play a crucial role in targeting immune responses and adaptive immunity. However, their ability to respond to cancer cells is often limited by tumor evasion tactics. Tumors impose severe glucose restrictions, creating intense competition for this critical nutrient, which is necessary for effective T cell function. Currently, adoptive T-cell transfer therapies have emerged as viable therapeutics but are hindered by the immunosuppressive nature of tumor environments. T cell activity and survival depend on metabolic reprogramming and upon activation there is an increased need for glucose. In the tumor microenvironment, glucose is limited, and T cell responsiveness is limited, resulting in immune evasion and cancer progression. Every year, an estimated 1.9 million people are diagnosed with cancer in the United States, many of whom could benefit from improved immune-based treatments. As the demand for innovative cancer treatments grows, the immunotherapy market continues to expand rapidly. In 2023, the global cancer immunotherapy market was valued at $119 billion and is projected to reach $198 billion by 2030.
Researchers at the University of Florida have developed glucose transporter overexpressing T-cells to enhance the metabolic fitness of T cells. This therapy addresses the glucose restrictions in the tumor microenvironment, where tumors consume most of the glucose and release high levels of lactate, suppressing T-cell function. Leveraging insights into tumor and T-cell metabolism, an additional therapeutic strategy reprograms T cells to interpret lactate as a positive signal, boosting glycolysis, activation, and tumor-targeting capabilities.
Boosts T cell glucose uptake to improve survival and tumor-targeting, offering potential breakthroughs for brain tumor patients, especially those with high-grade gliomas
T-cells play an important role in targeting immune response and adaptive immunity. However, their ability to respond to cancer cells is limited by tactics employed by tumors to evade the immune system, particularly glucose restriction. Available therapies focus on targeting tumors through external interventions like surgery, and chemotherapy. However, these can carry serious side effects and are less suitable for metastatic or widespread cancers. Traditional immune therapy is quite promising, using the body’s natural defenses to fight cancer, is limited by the complex immunosuppressive tumor microenvironment. Researchers at the University of Florida have developed a glucose transporter overexpressing T-cells to bypass the immune evasion that the tumor microenvironment promotes. This therapy modifies T-cells to increase glucose uptake, enabling them to survive and function in the nutrient-limited tumor microenvironment. Additionally, it reprograms T-cells to interpret lactate, a byproduct of tumor metabolism that usually suppresses immune function as a signal to enhance T-cell glycolysis, activation, and tumor targeting. These approaches improve the metabolic fitness of T-cells, helping them overcome glucose competition and immunosuppression in tumors.